

The Quiet Crisis Growing in Men's Health
By: Silke Schoch, MA, Director of Research & Programs
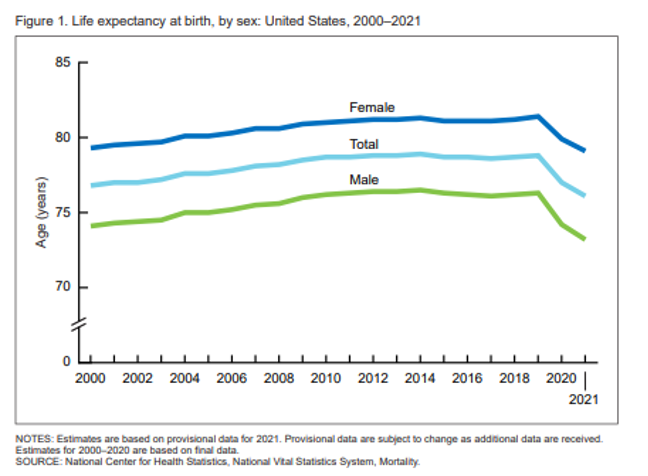
June is Men’s Health Month and spotlights the unique challenges that men and boys face in their health. A man living in the U.S. can expect to live 5.9 years less than the average American woman according to the Centers for Disease Control and Prevention (CDC) – 73.2 years (male) vs. 79.1 years (female). This goes even to the earliest health outcomes where mortality rates have increased for male infants in recent years. In 2022, the mortality rate was 6.06 for male infants vs. 5.12 for female infants. When looking at chronic conditions such as cancer, men are getting diagnosed at a higher rate than women in the United States, with non-Hispanic Black men having the worst rate of new cancer diagnoses. This same disparity is also reflected in the death rates for cancer with non-Hispanic Black men shouldering the heaviest mortality burden.
In both physical and mental health men are suffering. The American Foundation for Suicide Prevention found that, in 2022, “men died by suicide 3.85 times more than women.” The National Institute on Drug Abuse has done research that has shown, “[m]en are more likely than women to use almost all types of illicit drugs, and illicit drug use is more likely to result in emergency department visits or overdose deaths for men than for women.” Men tend to drink alcohol more than women which caused 3 million deaths in men worldwide in 2016. These are serious health conditions that interplay with mental health. Access to effective treatment can be worse in certain communities and research that has found that “Blacks, Latinos, and American Indians experience consequences for their substance use and substance use disorders disproportionately compared with those suffered by their White counterparts.” Patients living in rural communities also face significant barriers to finding treatment and are much less likely able to acquire medications that assist in opioid use disorder treatment.
Causes of these health inequities stem from a multitude of factors ranging from personal to societal. These include “biological vulnerabilities (which put [men] at a higher risk for developing rare disorders); societal and cultural factors, such as masculinity and risk-taking behaviors…and health care systems/institutional deficiencies, such as neglecting men’s mental health and emotional well-being.”
There are currently a number of initiatives in the U.S. that address the health of men and boys. Healthy People 2030 has a set of objectives specifically for the male population that includes prostate health and infection control improvement. The Patient-Centered Outcomes Research Institute has also funded projects that focus on men’s health including the “Community Health Alliance for Men’s Health Promotion (CHAMP).” However more work can be done, and the research community must have a shift in perspective that addresses men’s health inequities.

