CLINICAL OUTCOME ASSESSMENTS: BUILD NEW OR ADAPT OLD?
By Aimee Lee Russell, Associate, Programs
On Thursday, October 10, Stacie Hudgens, MA, Chief Executive Officer & Strategic Lead at Clinical Outcomes Solutions spoke about how to determine whether existing clinical outcome measures can be adapted for use or if a new tool should be designed from scratch. This was the 11th webinar in the NHC’s Clinical Outcome Assessment (COA) series.
Ms. Hudgens emphasized that it is important to capture outcomes that matter to patients in clinical outcome assessments. To be truly patient-centered requires engaging with patients at every stage of the development process. Each patient has unique goals, which may change as the nature of their condition evolves. Ms. Hudgens gave examples of patients with psoriasis – a skin condition where cells build up and form scales and itchy, dry patches – and how new biologics can be injected to better treat moderate to severe symptoms. But many patients do not want to try them because they prefer topical treatments that they have been using for a long time. By asking patients what matters most to them, clinicians and researchers can develop better studies and products that patients will use.
Ms. Hudgens elaborated on one type of clinical outcome assessment, patient-reported outcomes (PRO). A PRO is a report that comes directly from the patient without any interpretation or amendment by someone else. It is very important to engage patients before deciding what the PRO you use will be to learn what matters to them. After hearing from patients on the outcomes that they really care about, you can search through existing PROs see if there are any that measure the concept of interest you are focusing on.
Existing measures can be found by conducting a literature search and looking at the FDA’s COA compendium to identify COA tools you might consider for your study. There are many outcomes to study, but it is of utmost importance to keep the patient perspective in mind. What matters to researchers might not be as important to patients and vice versa.
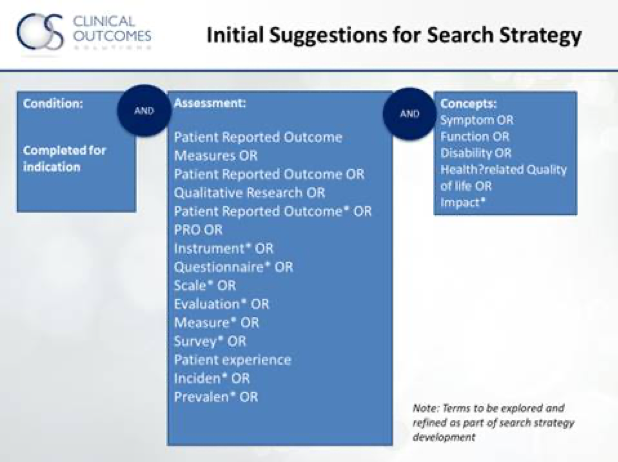
Below are common terms to begin your literature search to ensure the outcomes you evaluate are patient-centered.
If you do find a tool that measures the concept you are interested in studying, be sure that it is patient centered, or one that matters to patients. If the tool does not capture a patient-centered measure, it will need some modification. If there are no older, existing tools that fit what you are looking to study, you might consider building a new COA, that incorporates patient-centered methods and endpoints. Know that the process will take time and resources, but the end result will be a measure that captures the patient perspective. The diagram below can help guide you:
Ms. Hudgens stressed the importance of starting any study process by speaking with patients and caregivers to determine outcomes and measures that are most important to them. From there, you can judge whether existing COAs can be used or whether to adapt one or build a new tool.
You can view Ms. Hudgens’ full presentation here.