Existing Data
Seeking Existing Patient Impact Data
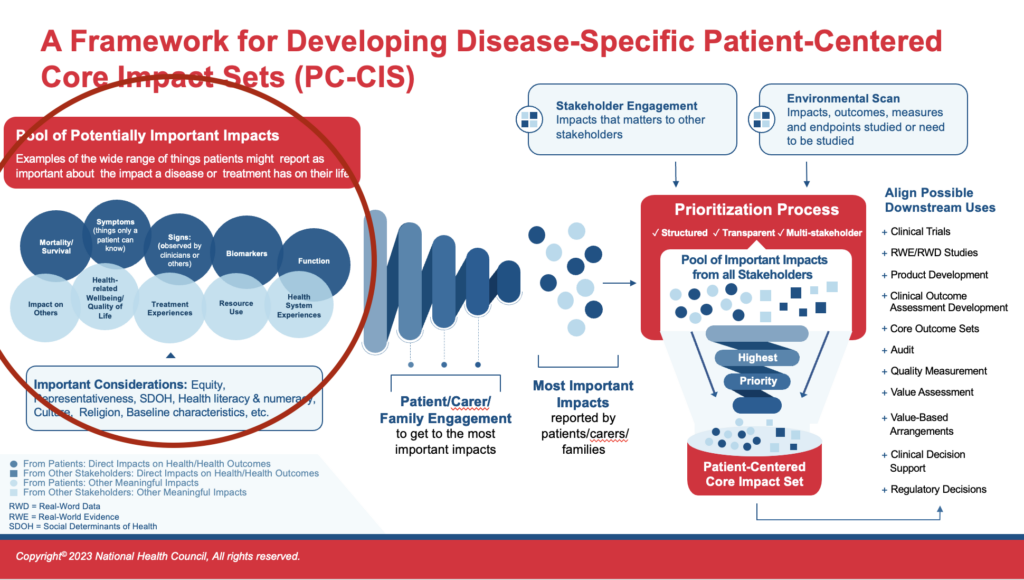
Within some disease communities or populations, previous efforts have already amassed data from which the impacts most important to patients could be gleaned. That is, information has likely already been collected directly from patients across many conditions, about what they identify as important about their disease(s) and/or treatments. This data gathering does not include information on what other stakeholders (e.g., clinicians, researchers) have identified as important to patients, which also might exist, but is addressed at a later phase in the process.
Patient-reported information can exist in a variety of formats and types such as qualitative research projects, Voice-of-the-Patient Reports, registries, social media listening, and publications. To date, this type of information will only rarely be found in a peer-reviewed publication. This paradigm shift, to beginning with patient-generated data rather than beginning with peer-reviewed literature, may require some flexibility and creativity to locate existing sources.
Examples of existing patient-provided impact data on an array of conditions include:
- S. Food and Drug Administration (FDA) Patient-Focused Drug Development (PFDD) website
- Disease-specific, patient-group led Voice-of-the-Patient Reports identified on patient group websites, e.g. National Kidney Foundation, Arthritis Foundation.
- Disease-specific registries such as RARE-X Patient-Powered registry or Duchenne Data registry
- Patient-Focused Medicines Development’s (PFMD) Synapse, includes information on engagement initiatives around the world
- The Core Outcome Measures in Effectiveness Trials (COMET) database has initiatives that include some patient-generated data
One potential source of existing patient impact data is a previously developed Core Outcome Set (COS). Whether or not a COS can be readily translated into a PC-CIS is not easy to determine and depends on how patient centered the existing COS is, how comprehensive the data gathering from patients was when capturing the outcomes considered, and if the prioritization process kept the patient voice intact. An existing Core Outcome Set that is highly patient centered may be an ideal data source for a Patient-Centered Core Impact Set. Others may require significant adaptation and others might not be useable at all. Each must be assessed on a case-by-case basis.
Evaluating Existing Impact Data Reported by Patients
Existing data will need to be evaluated by patients and other members of the PC-CIS team to determine if it is patient centered enough to be considered as a sound starting point. That is, you will need to evaluate whether or not what has been collected in the past captures what is important to the patient community from the patient community perspective. In some cases, the description of a project or effort does not provide enough detail to evaluate the patient-centered aspects or relevance and representativeness. It may be worth having a conversation with the patients and/or project leads (which may be the same people) who were involved to better understand how data were captured. You also will need to assess whether the data are recent enough to still be relevant. For example, if therapy for a specific condition has changed dramatically over the past decade, it would be important to have data that is reflective of patients’ experiences with the current suite of therapeutic options.
Another key consideration is the quality and rigor of the data collection. Some stakeholders harbor misconceptions about the characteristics of patient data and data collection by patient groups, making assumptions about poor methodology or other shortcomings. The “Is It Good Enough?” guide is a checklist for evaluating the quality and patient centeredness of existing data collected from patients.
Additional guidance for assessing patient centricity, quality, and representativeness of data includes:
- The National Health Council Rubric to Capture the Patient Voice
- The National Health Council Representativeness Rubric and Roadmap
- The Core Outcome Set – STAndards for Reporting (COS-STAR) guidance to describe geographic diversity of stakeholders.
The Outcome Measures in Rheumatoid Arthritis Clinical Trials (OMERACT) Handbook Principles, Chapter 3, Section C
Arthritis Use Case
- The Foundation had already amassed a significant amount of data from prior specific efforts and years of community programming. Among the specific initiative data sets were two externally-led Patient-Focused Drug Development (PFDD) meetings with Voice-of-the-Patient reports (one on osteoarthritis and one in Juvenile Idiopathic Arthritis ), the rheumatoid arthritis biologic survey conducted for an Institute for Clinical and Economic Review (ICER) review, a series of local and national listening sessions with an array of patients and family members, multiple research work groups conducted in partnership with the Childhood Arthritis and Rheumatology Research Alliance (CARRA), and outputs of from a Patient-Centered Outcomes Research Institute (PCORI)-funded Engagement Award to develop a patient-driven research agenda.
- In addition to these sources, the Arthritis Foundation had many years of evaluation data from conferences and local events through which patients and families expressed what they most needed and wanted for disease management and overall quality of life.
- Again, as the INSIGHTS program was not itself an effort to develop a PC-CIS, it did not “use” this data in the same way, but the work nonetheless involved leveraging existing data and most importantly beginning with patient-generated data versus beginning with existing published literature on outcomes or outcome sets.